Whenever a person realises that they are bleeding, it gets their attention. It’s usually easy to find the source of the blood, but when it’s coming from your rectum, the origin isn’t as easy to pinpoint. That’s enough to make anyone worry. So, what are the most likely sources of rectal bleeding?
Let’s quickly discuss the likely causes of rectal bleeding and what your next steps should be if it happens to you.
Welcome to another wonderful instalment of Ndlalane Health newsletters. I go by the name DocSakhi for many people but my government name is Sakhile Ndlalane, and I’ll be your guide on today’s topic. Let’s get to it.
Rectal bleeding can happen for many reasons, the vast majority of which are benign. The following steps can help you to determine if you need to be in contact with a doctor or not.
Your first task: Determine if you’re actually bleeding.
Before worrying too much about what you’re seeing in the toilet or on your toilet paper, think carefully about what you’ve eaten in the recent past. There are several foods and medications that can change the colour of your stool. For example if you ate beetroot, cranberries, tomatoes and products that use red food colouring.
Blueberries, black licorice and medications that contain bismuth — like Pepto Bismol® or Kaopectate® — can turn your stool black.
If you’ve confirmed that you are actually bleeding, your next step is determining the blood’s origin point. That can help you to figure out if you need to seek medical attention.
Blood color is one way to narrow down the possible causes of your rectal bleeding. Think of the blood color as indicative of travel time. It takes longer for blood from your esophagus to pass through your entire digestive system than blood from an anal fissure or closer to the lower end of the system. During travel time from upper digestive system to lower ends, the color and consistency of the blood changes. The redder the blood, the closer to your anus the origin point will be. In other words:
Bright Red blood - originates from your lower GI tract — think lower colon, rectum or anus.
Dark Red blood or Maroonish - originates higher up — think upper colon or somewhere in your small intestine.
Dark, tar colored blood - could originate as far up as your esophagus, it could be difficult to know you are bleeding in this instance, so it’s important to eliminate the possibility of food coloring.
Common causes of rectal bleeding
1. Hemorrhoids - It’s normal for everyone to have hemorrhoids inside and outside of their anus, and there are several reasons they may become irritated. If you notice blood on your toilet tissue or in the toilet, the factors that may point to hemorrhoids include:
· Constipation.
· Diarrhoea.
· Low-fiber diet.
· Heavy lifting.
· Hard stools.

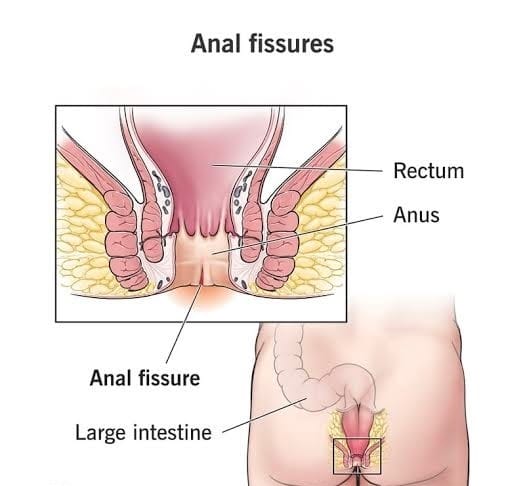
2. Anal Fissures - If there are tears in the tissue of your anus, then you may experience both rectal bleeding and pain during and after a bowel movement. Typical causes of anal fissures include:
· Chronic constipation.
· Diarrhea.
· Straining.
· Anal intercourse.
· Toys and gadgets inserting
3. Diverticulosis and Diverticulitis - When tiny pockets, or diverticula, form in the lining of your bowel, you have diverticulosis. Pressure on weak spots in your intestinal wall may cause these tiny pockets to form. Diverticulitis occurs when your diverticula become infected and swollen.
4.Peptic ulcers - a peptic ulcer occurs when gastric acid eats away at the protective walls of your stomach. The resulting sores frequently bleed.
Inflammatory bowel diseases - conditions like ulcerative colitis and Crohns disease inflame your intestines. Blood loss can be mild, but it can also be significant enough to cause anaemia.
5. Colon cancer - In a very small number of cases, rectal bleeding is a sign of colon cancer. You may also notice other symptoms, such as unexplained weight loss or pain in your abdomen.
Colon cancer typically starts with polyps in your colon. Early detection is the goal here. Polyps are typically benign at first, and a surgeon can remove them before they become cancerous if you catch them early. Medical screening is very important, especially for cancer.
I have said too many medical jargon that I struggled to simply but mostly I can emphasise that hemorrhoids and anal fissures are responsible for rectal bleeding about 98% of the time. But it’s important to let your doctor know if you experience rectal bleeding so they can rule out any other problems.
I hope you are still following. I really thought this would be a short discussion but I realize that there is so much to tell you. In the spirit of our theme and motto, #BeInTheKnow. Let’s try to proceed 😊.
Painful rectal bleeding
Painful rectal bleeding, while certainly unpleasant, isn’t always a sign that something’s seriously wrong. A lot depends on the severity of the pain and where you’re feeling it. Hemorrhoids and anal fissures can hurt. In most cases, though, they either spontaneously resolve themselves or are easily treated by your doctor. Pain or cramping in your abdomen is a different story. If you’re in significant pain, regardless of the cause, you should speak with a doctor.
Rectal bleeding with no pain
It may be preferable, but painless rectal bleeding isn’t necessarily less severe than painful rectal bleeding. Hemorrhoids aren’t always painful, but the same is true of colorectal cancer. Not being in pain isn’t a reason to skip a trip to the doctor, especially if you have other symptoms, like changes to your stool or nausea.
How to manage bleeding at home
If you’re fairly certain that the bleeding is the result of hemorrhoids or an anal fissure, you don’t need to run to the doctor. These are common problems, and you can treat them yourself at home.
Use an over-the-counter medication: There are lots of hemorrhoid creams, ointments and suppositories available at your local drugstore. Don’t use steroid creams.
Use medicated wipes: Witch hazel-soaked pads work as an astringent, cleaning your anus and reducing itching and irritation.
Use an ice pack for pain relief: If the idea of grabbing an ice pack from your freezer squeaks you out, you’re not alone. Luckily, there are ice wedges designed for hemorrhoid care that — like perineal ice packs — come with washable sleeves. If you suffer from chronic recurring hemorrhoids then it’s worth the consideration
Take a sitz bath: If you’re struggling with pain, burning or itching, it’s time to get in the tub. This shallow-warm water bath will increase blood flow to your anal tissues, which will facilitate pain relief and healing.
Bathe daily: This might sound strange, reminding people to bath everyday but it might not even suprise you that, we don’t exactly bath everyday but if you’re struggling with hemorrhoids or fissures, it’s important to keep the skin around your anus clean. Remember to steer clear of harsh soaps that could irritate the area further.
There are also things you can do every day to prevent hemorrhoids and anal fissures.
Stay hydrated: That means drinking enough water. I always get asked, the question of how much is enough water. I hope I can settle that question here, now and for all. Take your total weight and multiply it by 40ml then you get the amount you need to Hoover around in a day. Remember this is your total fluid intake, including water in food and other beverages. Example if you weigh 65kg it will look like this; 65 x 40 = 2600ml which when divided by 1000 ml gives you 2.6 litres of water. It’s ok if you don’t finish the entire 2.6 litre because you eat as well which also has fluids. The idea is to Hoover around those figures:numbers in terms of your daily intake. It also means limiting your alcohol and caffeine intake.
Avoid straining and sitting on the toilet too long: It puts pressure on the veins in your rectum and anus, which can cause new hemorrhoids to form — or exacerbate the ones you already have. One this is to avoid going there with your phone, so that you don’t seat there longer than necessary.
Increase your fiber intake: Constipation and hard stools can cause hemorrhoids and anal fissures. A high-fiber diet will soften your stool, which, in turn, keeps you from straining.
Lastly, this is slightly more tempering with people’s sexual preferences but please avoid anal intercourse when it’s possible.
If these home remedies aren’t alleviating your symptoms, or you’re continuing to bleed, it’s time to get medical attention.
When to see a doctor
Because rectal bleeding has so many causes — some routine, others rare — it’s important to pay close attention to the kind, severity and duration of the symptoms you’re experiencing. Those factors determine the type of medical attention you need and the urgency with which you need it.
Schedule a visit with a doctor if the bleeding lasts more than one to two days or if symptoms haven’t improved after trying home remedies for a week.
Get immediate medical attention if the bleeding is continuous or heavy, or if you’re experiencing the following symptoms:
Nausea.
Vomiting.
Diarrhea.
Abdominal pain or cramping.
Narrow stools or a change in the quality or frequency of your stools.
Call an ambulance or rush to the nearest hospital if you’ve lost more than two pints of blood,(this is blood loss over a litre). If you sustained severe rectal trauma like a puncture wound or you’re experiencing the following symptoms of shock:
Rapid, shallow or difficult breathing.
Dizziness or blurred vision.
Lightheadedness or fainting.
Confusion.
Remember, no matter where it’s coming from, blood loss exceeding two pints is a serious medical emergency. Losing more than 4.2 pints of blood is potentially deadly. If your bleeding is that severe, you need an ambulance.
What your doctor needs to know
It’s helpful if you can make a note of how long you’ve been experiencing rectal bleeding, if it stops then starts again and how long it lasts.
Your doctor will likely ask you:
Do you see the blood in the stool and/or in the toilet bowl?
What color is the blood?
Does the blood always show up with a bowel movement?
What other symptoms (if any) are you experiencing?
Are you in pain?
What is your family medical history?
Ok we have discussed too much information in such a short space of time, let’s conclude🧘🏽♂️.
Thank you for reading up to this far. I would love to hear your thoughts and feedback on this article. You can simply reply to this article or send me an email to [email protected]
Before I go, here is a carry pack; Plan to start screenings after the age of 45
Even if you aren’t experiencing problems or noticing any rectal bleeding, it’s vital to begin having colorectal cancer screening once you are 45 years and older. Sometimes earlier if you are suffering from chronic rectal bleeds. Please start earlier if there a history of rectal cancer in your family. Whenever possible, you should start getting colonoscopies 10 years before the age at which your relative received their cancer diagnosis).
In closing, remember It’s not unusual to be squeamish about butts and guts, but neither is it unusual to have problems with them.
Rectal bleeding is a common medical issue that’s usually harmless but can also be a warning sign for something much deadlier.
When in doubt take a glass of water, it can help you to swallow your pride with ease 😂 so that you can go talk to your doctor about these things.
It’s better to be safe than sorry.
That’s it for today. Happy weekend. Cheers bye for now. ✌🏽